Big Data, Small Payoff: Madrid Study Finds Pediatric mRNA Vaccine Benefits Thin—and Safety Questions Still Linger
The new ACIP made the right call; if anything, it was too conservative.
trialsitenews
TrialSite Staff | Making Biomedical Research Evidence Accessible to All
Dec. 31, 2025, 4:30 a.m.
A massive real-world study from Madrid looked at millions of children’s medical records to answer a simple question parents care about: did COVID-19 vaccines clearly protect kids from serious illness—and were they safer than doing nothing? The answer was not reassuring. Serious COVID outcomes were already very rare in children, and vaccination reduced hospitalizations by only a handful per 100,000, mainly in teenagers. For younger children, the benefit was minimal and uncertain. Safety problems like heart inflammation were uncommon—but did not clearly disappear in vaccinated teens. The findings challenge the logic of one-size-fits-all pediatric vaccine policies. Do the outcomes potentially contribute to the move recently by the Centers for Disease Control and Prevention (CDC) Advisory Committee on Immunization Practices (ACIP) in moving away from the universal COVID-19 vaccination?
TrialSite Executive Overview
Led by Miguel A. Hernán, MD, of Harvard T.H. Chan School of Public Health, this population-based study—“Effectiveness and Safety of COVID-19 mRNA Vaccines in Children 6–17 Years Old,” published in The Pediatric Infectious Disease Journal—used Madrid’s region-wide health registries to emulate a randomized “target trial.” Analyzing 460,834 vaccinated children and 2,304,170 matched controls, investigators asked whether mRNA vaccines meaningfully reduced COVID-19 hospitalization, MIS-C, and myocarditis/pericarditis. The results were sobering: benefits were small and age-dependent, severe outcomes were rare regardless of vaccination, and safety signals—though uncommon—were not clearly lower in vaccinated adolescents. These findings directly challenge assumptions behind universal pediatric COVID-19 vaccination.
Study Design
This population-based observational study emulated a target trial using linked Madrid Health System registries covering nearly the entire population. Children aged 6–11 and 12–17 were matched 1:5 (vaccinated to unvaccinated) by age, sex, postal code, and calendar time. Outcomes were tracked for 240 days and restricted to COVID-19 hospitalizations where COVID-19 was the primary cause, multisystem inflammatory syndrome in children (MIS-C), and acute myocarditis/pericarditis. Analyses focused on per-protocol effects. The study reported no industry funding and received regional ethics approval.
Findings
Ages 6–11: COVID-19 hospitalization was extremely rare—about 12.7 per 100,000 in unvaccinated children over 240 days. Vaccination reduced this by 1.2 per 100,000, an estimated 9% effectiveness with wide confidence intervals that included no benefit. No myocarditis or pericarditis cases occurred in either vaccinated or unvaccinated children. MIS-C was also rare, with differences too small to be reliable.
Ages 12–17: Vaccine effectiveness against COVID-19 hospitalization was higher but still modest: 45% relative reduction, equal to 5.3 fewer hospitalizations per 100,000. Myocarditis/pericarditis occurred at similar rates in vaccinated and unvaccinated adolescents (about 7–8 per 100,000), yielding a risk ratio of 1.09 with wide uncertainty. MIS-C remained rare in all groups.
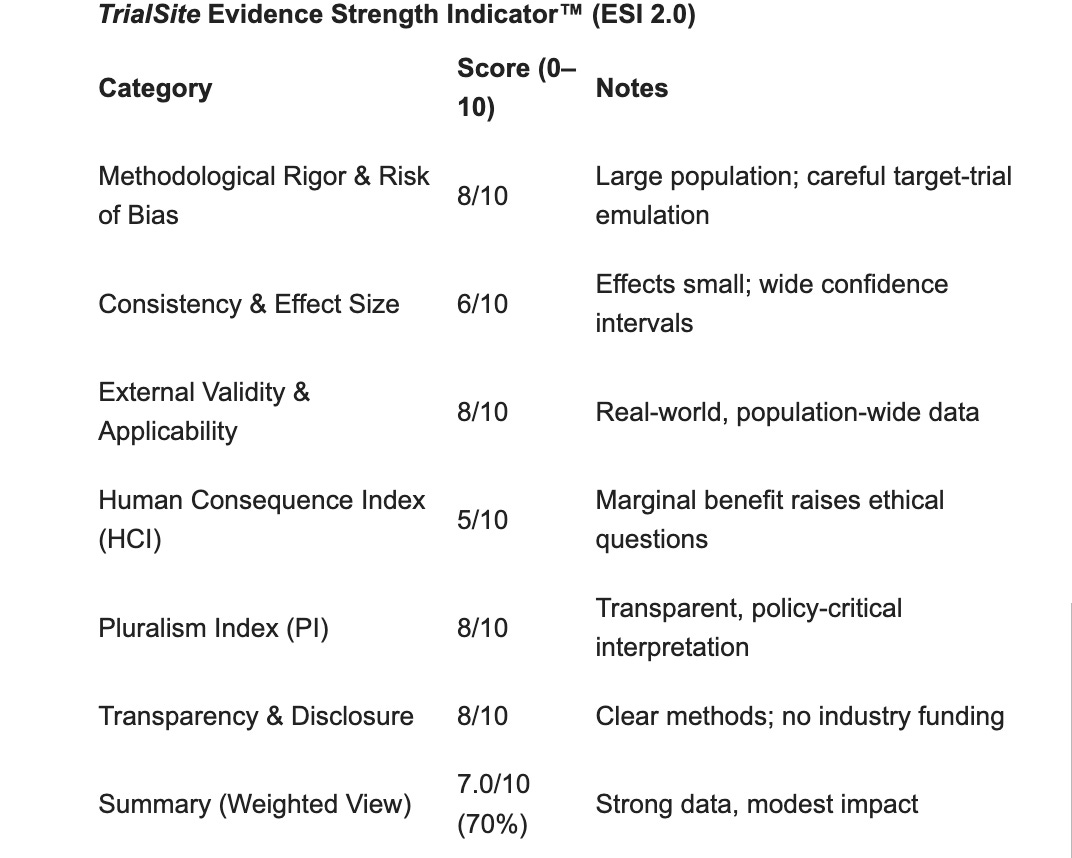
Red Flags & Limitations (TSN ESI 2.0)
What should concern us all
Tiny absolute benefit. Even where vaccines “worked,” they prevented only a few hospitalizations per 100,000 children.
Wide uncertainty. Confidence intervals often included minimal or no benefit, especially in younger children.
Safety not clearly improved. Heart inflammation was rare—but not demonstrably lower in vaccinated teens.
Methodological limits include observational design, potential unmeasured confounding, and no assessment of long-term outcomes.
Human Consequence Index (HCI): Raises proportionality and informed-consent concerns when benefits are marginal.
Pluralism Index (PI): Strong—authors openly acknowledge low event rates and policy uncertainty.
Conclusion & Implications
This Madrid study provides moderate-strength evidence that both the benefits and risks of mRNA COVID-19 vaccination in children are small, particularly for ages 6–11, where severe COVID-19 outcomes were already rare. For policymakers, the data support moving away from universal pediatric mandates toward individualized, risk-based decisions.
In summary:
This study shows limited real-world benefit, low but persistent safety concerns, and the need for more restrained, transparent pediatric vaccine policy.
Citation: Hernán MA, Álvaro-Meca A, Calvo-Alcántara MJ, et al. (2025). Effectiveness and Safety of COVID-19 mRNA Vaccines in Children 6–17 Years Old: A Population-Based Study in Madrid. The Pediatric Infectious Disease Journal.
Journal Impact Factor: 2.2
© 2025 TrialSite News™. All rights reserved. Republished by permission and request.



I wish somebody would stop being so polite and come out and say it.
The big pharma cartel along with their deep state buddies (fauci et al) created a problem, promoted it as an existential threat and then sold us some expensive, ineffective snake oil as the ONLY possible cure (there were several other viable choices that were intentionally buried or otherwise made unobtainable) and in the process profited many BILLIONS of dollars.
Gratitude, Dr. Malone for your mission to protect and safeguard the public trust with truthful, scientific and straightforward reports.